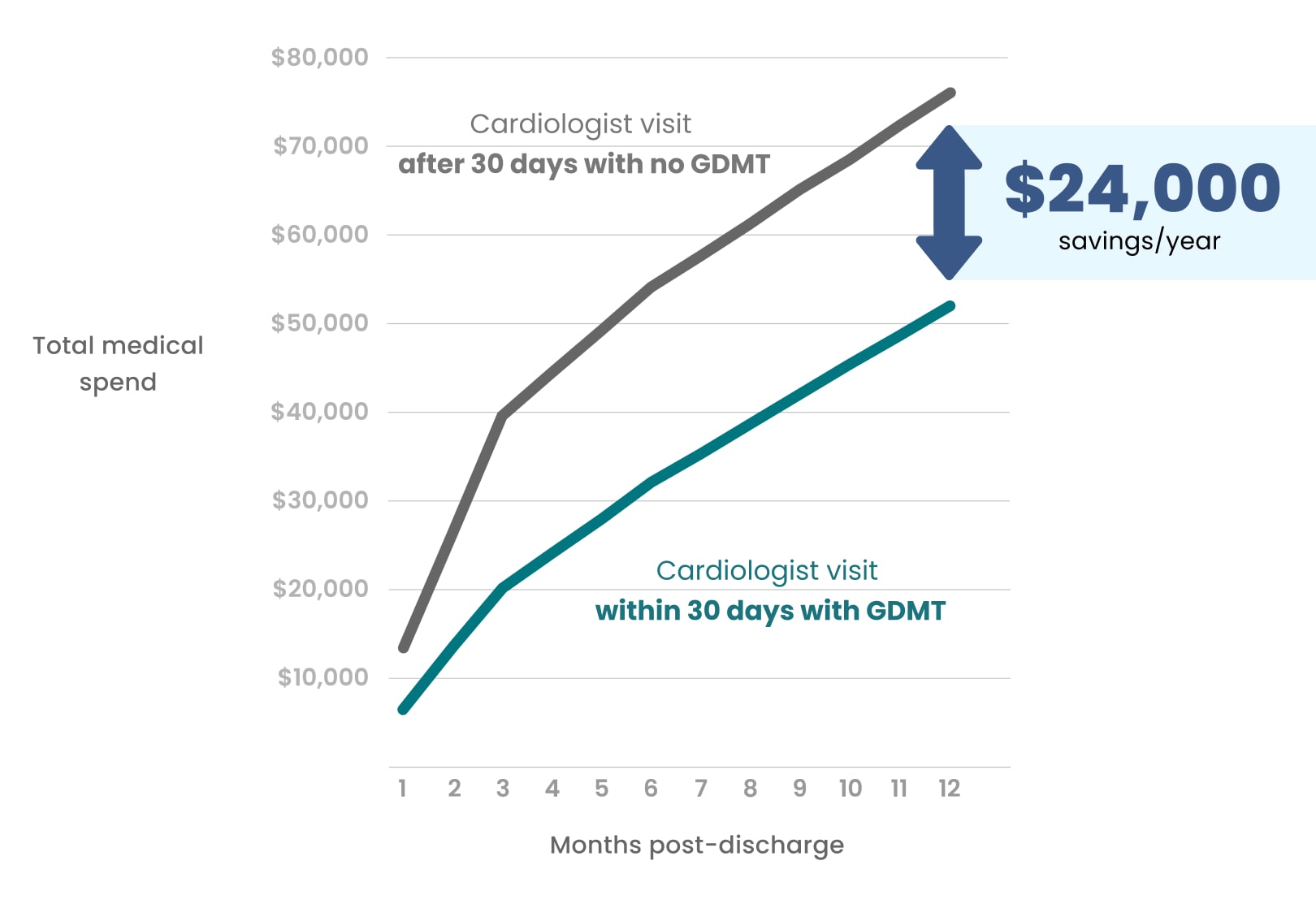
By increasing access to cardiac care and proven therapies, we improve patient outcomes and drive savings for our partners.

By increasing access to cardiac care and proven therapies, we improve patient outcomes and drive savings for our partners.
1New Onset Heart Failure diagnosed in Inpatient Setting – Medicare FFS Claims Data, 2021, CA, NC, WI, PA, KY (population adjusted average), n=21,590 22023, North Carolina, Medicare FFS Claims data (n=16,437) 3AMN Healthcare 2022 Survey of Physician Appointment Wait Times and Medicare and Medicaid Acceptance Rates. (2022). [Survey]. AMN Healthcare. https://www.amnhealthcare.com/blog/physician/perm/physician-appointment-wait-times-getting-longer/ 4Greene SJ, Butler J, Albert NM, et al. Medical Therapy for Heart Failure With Reduced Ejection Fraction: The CHAMP-HF Registry. J Am Coll Cardiol. 2018;72(4):351-366. doi:10.1016/j.jacc.2018.04.070